Abstract
Objectives: Primary central nervous system lymphoma (PCNSL) is a rare aggressive B-cell lymphoma, particularly in HIV-negative individuals, that represents a clinical challenge due to its location and lack of comprehensive molecular and biologic description. Histopathologic features are that of diffuse large B-cell lymphoma with expression of pan-B-cell markers as well as cell of origin (COO) germinal center B cell (GCB) and post-germinal center B cell (non-GCB) markers. Previous studies using immunohistochemistry (IHC) suggest that the majority of PCNSL cases are non-GCB. However, gene expression profiling has revealed non-GCB to be comprised of two distinct subtypes, namely activated B-cell (ABC) and unclassified (UNC) subtypes that are indistinguishable by IHC. To date COO testing using the highly accurate Lymph2Cx gene expression profiling assay has not been reported in PCNSL.
Methods: IRB approval was obtained and HIV negative patients diagnosed with PCNSL, who had given informed consent and for whom archived tumor tissue was available for testing were identified. COO testing was performed using the Lymph2Cx NanoString assay on RNA extracted from formalin-fixed, paraffin embed tissues using our established laboratory protocols. Clinical data including patient demographics, lines of treatment and survival outcomes were collected and correlated with each other and Lymph2Cx COO results.
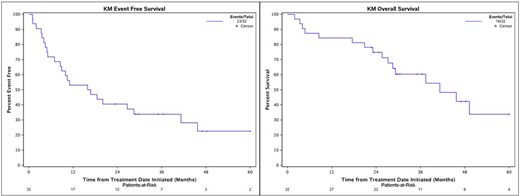
Results: Thirty-two HIV-negative patients diagnosed between January 2005 and June 2015 were included. Median age was 61 years (30-82) and 53% were male. Radiographic information was available for 18/32 patients. Eleven (61%) had a single brain lesion at diagnosis, while 7 (39%) had >1 brain lesion. Lines of systemic therapy were 1 (91%) and 2 (9%). All patients received methotrexate-based induction therapy (44% received methotrexate, rituximab and temozolomide, 16% received single-agent methotrexate, 31% received methotrexate and rituximab, and 9% received the modified Bonn regimen; methotrexate and cytarabine-based induction). A total of 10 patients (31%) received high-dose chemotherapy and autologous stem cell transplant (ASCT) for consolidation. Of the 10 patients that underwent consolidation therapy, 9 underwent ASCT after first line induction, and 1 underwent ASCT after second line therapy. None of the patients received whole-brain radiation therapy. At a median follow-up of 29 months (range of 2-107) median event-free survival (EFS) was 16.3 months (95% CI, 8.8-45.7), and median overall survival (OS) was 41.2 months (95% CI, 28.5-NE).
COO testing using the Lymph2Cx assay revealed that 91% (29/32) were ABC, 9% (3/32) were GCB, and none were UNC. Histopathology reports described COO using the Hans algorithm in 11 of the 32 cases. Of the 3 determined to be GCB on Lymph2Cx, 1 was denoted GCB by the Hans algorithm and 2 were not stained to determine COO. Of the 29 determined to be ABC by Lymph2Cx, 9 were denoted non-GCB and 1 was denoted GCB by the Hans algorithm, and 19 were not stained to determine COO.
Conclusions: This series of HIV-negative patients with PCNSL showed median survival consistent with previous studies. In this first series using the Lymph2Cx assay, we confirmed that over 90% of PCNSLs are of ABC subtype, which concurs with previous reports that PCNSL tumors are predominately non-GCB by the Hans algorithm. These findings provide biological rationale forthat pharmacologic interventions targeting B-cell receptor signaling to be explored in clinical trials in the majority of patients with PCNSL.
Rimsza:NanoString: Other: Inventor on the patent for the Lymph2Cx assay.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal